Beyond Reproductive Health: How Hormonal Therapy Shapes the Gut Microbiome
Hormonal therapy is a cornerstone in women's health, widely used for contraception, managing polycystic ovary syndrome (PCOS), polycystic ovary disease (PCOD), and alleviating symptoms of menopause. While the benefits of hormonal therapy are well-established, emerging research suggests that its influence extends beyond reproductive health, potentially affecting the gut microbiome—an essential yet often overlooked aspect of overall well-being.
In this blog, we explore the intricate relationship between hormonal therapy and the gut microbiome, shedding light on how this interplay may impact women's health.
Hormonal therapy involves the administration of hormones,typically estrogen and progesterone, to regulate or replace the body's natural hormone levels.
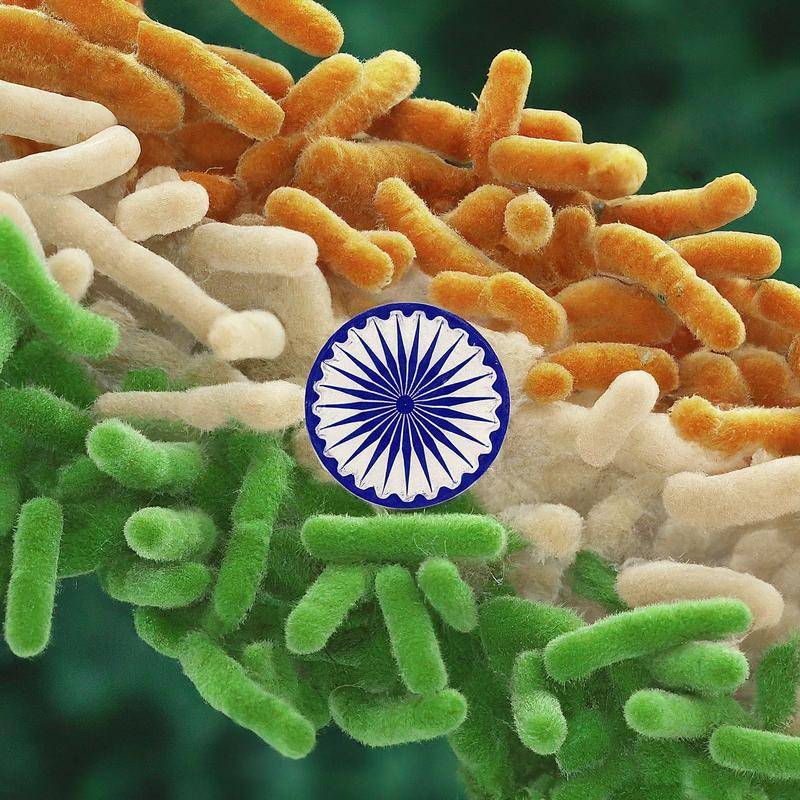
While hormonal therapies offer significant benefits, they may also influence the gut microbiome—a complex community of trillions of microorganisms that play a crucial role in digestion, immunity, and overall health. Research has shown that the gut microbiome is sensitive to various factors, including diet, lifestyle, and medications. Hormonal fluctuations, whether due to natural processes like menstruation or external interventions such as hormonal therapy, impacts the composition and function of the gut microbiome.
One study published in the National library of medicine found that women using hormonal contraceptives had a distinct gut microbiome profile compared to non-users. The researchers observed differences in the relative abundance of specific bacterial taxa, which may have implications for metabolic health and immune function.
The exact mechanisms underlying these changes are not fully understood, but it is hypothesized that hormonal contraceptives may influence gut permeability, immune responses, and microbial metabolism. These alterations could potentially affect nutrient absorption, inflammation, and susceptibility to gastrointestinal disorders.
PCOS is characterized by elevated levels of androgens, insulin resistance, and chronic low-grade inflammation—all of which can impact the gut microbiome. Women with PCOS have been found to have an altered gut microbiome composition, with reduced microbial diversity and an imbalance between beneficial and harmful bacteria.
A study published in the Journal of Clinical Endocrinology & Metabolism highlighted that hormonal therapy in PCOS patients could partially restore microbial diversity, suggesting a potential therapeutic benefit. However, the long-term effects of such interventions on gut health and overall metabolism remain an area of active research.
Menopause marks a significant hormonal shift, with declining estrogen levels leading to various physiological changes. Hormone replacement therapy (HRT) is often prescribed to alleviate menopausal symptoms, but its effects on the gut microbiome are still being explored.
Emerging evidence suggests that estrogen plays a role in maintaining gut barrier integrity and modulating the immune response. As estrogen levels drop during menopause, these protective effects may wane, leading to changes in the gut microbiome.
Further a study in a journal published by Multidisciplinary Digital Publishing Institute reported that postmenopausal women on HRT had a gut microbiome composition more similar to that of premenopausal women, with higher levels of beneficial bacteria such as Lactobacillus. This finding suggests that HRT may help counteract some of the adverse changes in the gut microbiome associated with menopause. But care should be taken before taking the hormonal therapy as when estrogen is given alone to a women with an intact uterus the chances of developing endometrial cancer increases hence estrogen is given in adjunct with progesterone or progestin.
In a nutshell, hormonal therapy is a powerful tool in managing various aspects of women's health, from contraception to menopause. However, its impact on the gut microbiome—a critical component of overall health—warrants further exploration. As researchers continue to unravel the complex interactions between hormones and gut microbes, it is becoming increasingly clear that maintaining a balanced gut microbiome is essential for optimizing the benefits of hormonal therapy.
Healthcare providers should consider the potential effects of hormonal therapy on the gut microbiome when prescribing these treatments and explore strategies to support gut health in women undergoing such therapies. By taking a holistic approach that integrates gut health with hormonal management, we can pave the way for more effective and personalized healthcare for women.
References
Association Between the Vaginal Microbiota, Menopause Status, and Signs of Vulvovaginal Atrophy