The Allergy Truce: Brokered by Your Gut
Do you sneeze through spring, swell up after eating peanuts, or break into hives for no apparent reason? You’re not alone. Allergies affect over 400 million people worldwide, and their incidence is rising faster than ever. While we usually blame pollen, dust, or food for our symptoms, emerging science suggests we may need to shift our focus inward—to our gut.
Yes, that’s right. The trillions of bacteria, viruses, and fungi living in our digestive tract—collectively known as the gut microbiome—may be playing a key role in shaping how our immune system reacts to allergens. This World Allergy Week, let’s explore the science behind this surprising connection.
What Exactly Is an Allergy?
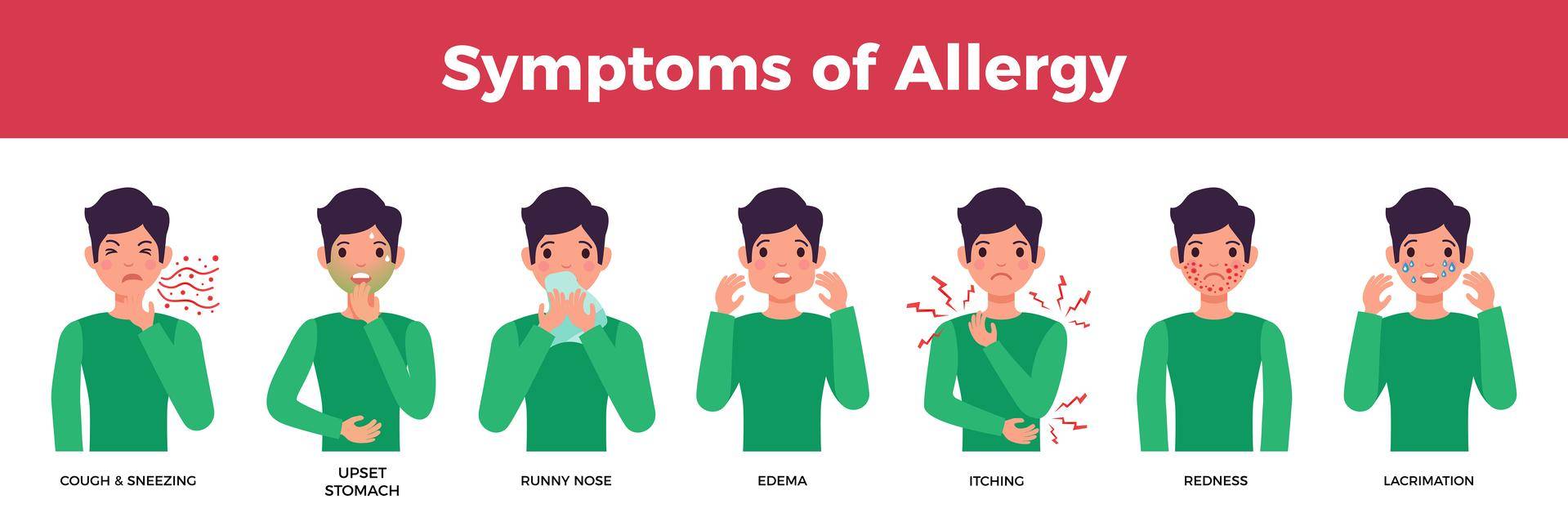
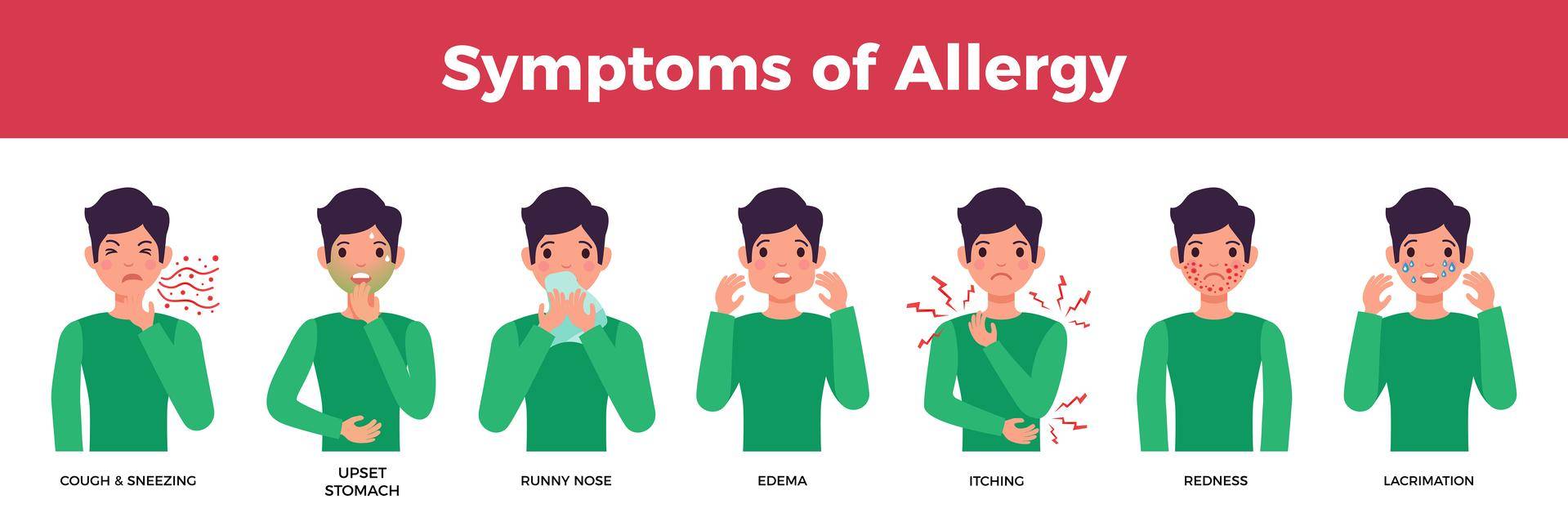
An allergy is essentially a case of mistaken identity by the immune system. It wrongly identifies a harmless substance (like pollen, peanuts, or pet dander) as a threat and mounts an exaggerated response. This “overreaction” leads to the release of histamines and inflammatory chemicals, which cause classic allergy symptoms—sneezing, itching, rashes, or even anaphylaxis in severe cases. But the real question is: Why does the immune system overreact in some people and not in others? That’s where your gut microbiome could have a hand!
Meet the Gut Microbiome: Your Inner Immune Coach
The gut microbiome is a bustling community of microorganisms that reside in our intestines. They’re not just passive passengers—they’re deeply involved in critical processes like digestion, vitamin production, and immune regulation. Here's how the gut microbiome influences allergies:
- Immune System Training:
Early in life, gut microbes help “educate” the immune system, teaching it to distinguish between friend and foe. A well-trained immune system ignores harmless substances and only responds to real threats like pathogens.
- Regulating Inflammation:
Gut bacteria produce short-chain fatty acids (SCFAs) like butyrate, propionate, and acetate, which have powerful anti-inflammatory properties. These SCFAs help maintain a balanced immune response and reduce the likelihood of hypersensitivity.
- Maintaining Gut Barrier Integrity:
A healthy gut microbiome strengthens the intestinal lining, preventing the leakage of undigested food particles and toxins that could trigger immune responses (a phenomenon sometimes called "leaky gut").
The Gut-Allergy Axis
Let’s break down the evidence that connects the gut microbiome to allergic diseases.
- Early-Life Microbiome and Allergy Risk
Numerous studies have shown that microbial diversity in infancy plays a crucial role in shaping immune tolerance. Babies delivered via cesarean section, fed formula, or given early antibiotics often have less diverse microbiomes and a higher risk of developing allergies.
- Microbiome Differences in Allergic vs. Non-Allergic Individuals
Adults and children with allergic conditions often show distinct microbial profiles. For example: Asthma patients often have increased levels of Clostridium and decreased Prevotella. Children with eczema have fewer beneficial bacteria like Lactobacillus and Bifidobacterium. Food-allergic individuals show reduced microbial diversity and increased gut permeability. These patterns suggest a dysbiotic microbiome—one that's imbalanced—may be linked to increased allergy susceptibility.
- The Hygiene Hypothesis: Too Clean for Our Own Good?
This theory suggests that modern lifestyles—marked by sanitization, processed diets, antibiotics, and urban living—reduce microbial exposure in early life, weakening immune training. People in rural environments or with pets and siblings (a.k.a. more microbe-rich settings) often have lower rates of allergies and asthma. It’s not about being dirty—it’s about being microbially diverse.
Can We Modify the Gut to Reduce Allergy Risk?
Here's the exciting part: our microbiome is malleable! While our early-life exposure sets the foundation, we can continue to nurture a healthy gut ecosystem through lifestyle choices. These include consuming a fibre-rich diverse diet that promotes microbial diversity and SCFA production, fermented foods that introduce beneficial microbes into your system, limiting highly processed foods, artificial sweeteners, and over the counter antibiotic use. Chronic stress is another offender that is increasingly being linked to gut dysbiosis and inflammation. Mindful practices, sleep, and movement also play a role in nurturing your gut-immune axis.
The Bottom Line
Your allergies may be more than skin-deep or nose-deep—they might be gut-deep. While genetics and environmental triggers play their role, your gut microbiome is a powerful immune regulator that can tip the balance between tolerance and hypersensitivity. Though more research is needed to define the exact microbes and mechanisms involved, one thing is clear: a diverse, well-nourished gut microbiome is foundational to immune health. This World Allergy Week, take a moment to appreciate your gut bugs. They may just be your best allies in the fight against allergies!
Read More Here:
- Role of the Microbiome in Allergic Disease Development
- The Role of Early Life Microbiota Composition in the Development of Allergic Diseases
- Delayed gut microbiota maturation in the first year of life is a hallmark of pediatric allergic disease
- Thinking bigger: How early-life environmental exposures shape the gut microbiome and influence the development of asthma and allergic disease
- The Microbiome as a Gateway to Prevention of Allergic Disease Development

